Table of Contents
As a geriatrician with over 15 years of experience, I’ve learned that the most profound lessons often come not from textbooks, but from the quiet moments of failure in a hospital room.
My most formative lesson began with Mrs. Eleanor Vance, an 84-year-old woman admitted from her nursing home for confusion.
Her case seemed straightforward, almost routine.
Her lab work showed a serum sodium of 124 mEq/L, a clear case of hyponatremia, or low sodium in the blood.1
I was confident.
The diagnostic flowchart I had memorized was clear: assess her fluid volume, find the cause, and correct the number.
The first step, assessing her volume status, was immediately challenging.
In older adults, the classic signs of dehydration like skin turgor or postural blood pressure changes are notoriously unreliable.3
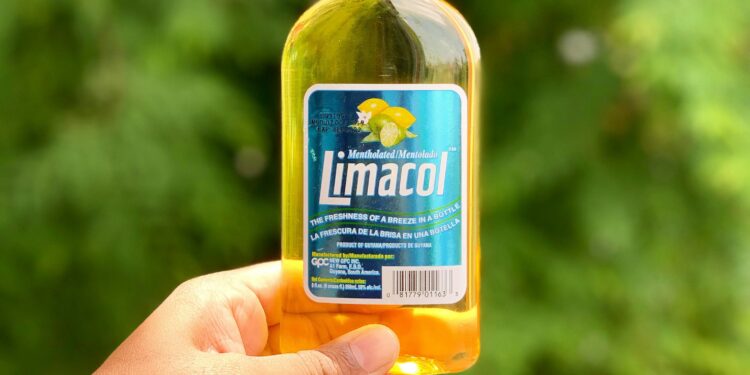
Based on a brief history from her caregivers about her limited diet, I settled on a diagnosis of “Tea and Toast Syndrome,” a form of low-solute hyponatremia common in the elderly, and classified her as euvolemic, meaning she had a normal fluid volume.5
Following the standard protocol for this diagnosis, I initiated a fluid restriction.2
But Mrs. Vance didn’t improve.
Over the next two days, her sodium level barely moved, and her confusion worsened.
I felt a growing knot of frustration.
Then came the call from the nurse that every physician dreads.
Mrs. Vance, more disoriented than ever, had tried to get out of bed on her own.
She had fallen and fractured her hip.
In that moment, the full weight of my failure crashed down on me.
I had followed the rules, checked the boxes on the algorithm, and yet, I had profoundly harmed my patient.
Her fall was a direct, devastating consequence of her untreated hyponatremia—a condition that we now know is a major risk factor for falls, fractures, cognitive decline, and even death in older adults.4
It forced me to confront a terrifying possibility: it wasn’t that I had misapplied the model; it was that the model itself was broken.
The conventional approach, with its illusion of simplicity, was dangerously inadequate for the complex reality of my geriatric patients.
Quick Answers: The Geriatrician’s Field Guide to Sodium Safety
My experience with Mrs. Vance set me on a new path.
For those navigating this complex issue, here are the core principles I learned, distilled from years of practice and research.
- Core Principle: Managing low sodium in an older adult is not about fixing a number. It is about becoming a “systems engineer” for the human body. You must first understand the patient’s entire biological control system—its aging components, its unique inputs, and its faulty signals—before making a single adjustment.
- Why is low sodium so dangerous in the elderly? Even mild, chronic hyponatremia is not a benign finding. It directly contributes to confusion, an unsteady gait, falls, and fractures, and is associated with increased mortality.9 It is a silent threat that is often tragically misattributed to “just getting old”.4
- What is the biggest mistake clinicians make? Oversimplifying the cause. Hyponatremia in older adults is rarely due to a single problem. It’s almost always a “perfect storm” of age-related physiological changes, multiple medications (polypharmacy), chronic diseases, and nutritional factors.4 Pinning it on one cause is a setup for failure.
- What is the safest approach? Think, then act slowly. A thorough diagnostic investigation to identify all contributing factors is mandatory before starting treatment. And when treatment begins, correction of the sodium level must be slow and cautious to avoid the life-threatening risk of osmotic demyelination syndrome, a form of brain damage caused by rapid fluid shifts.13
Part I: The Conventional Blueprint and Its Cracks
To understand why the standard approach failed Mrs. Vance, we must first look at the blueprint itself.
In medical school, we are taught to classify hyponatremia based on the patient’s total body water volume.
It’s a neat, logical flowchart with three main branches 1:
- Hypovolemic Hyponatremia: The patient has lost both water and sodium, but more sodium than water. This is typically caused by things like diuretic use, vomiting, or diarrhea.
- Hypervolemic Hyponatremia: The patient has gained both water and sodium, but more water than sodium. This is common in conditions like heart failure, liver cirrhosis, or kidney failure.
- Euvolemic Hyponatremia: The patient has a normal amount of sodium but an excess of water. The classic cause is the Syndrome of Inappropriate Antidiuretic Hormone (SIADH), where the body retains too much water.
This model promises clarity.
You determine the volume status, which points you to a list of likely causes, which in turn dictates the treatment.
For Mrs. Vance, I diagnosed euvolemic hyponatremia from “tea and toast” syndrome, so the treatment was fluid restriction.
It was logical, but it was wrong.
The problem is that in geriatric medicine, this clean blueprint is riddled with cracks.
Crack #1: The Unreliable Physical Exam
The very first step of the algorithm—assessing volume status—is built on shaky ground in the elderly.
The physical signs we rely on in younger patients are often misleading.
An older person’s skin loses its elasticity, making skin turgor a poor indicator of hydration.
Dry mucous membranes can be caused by medications or mouth-breathing.
And postural hypotension—a drop in blood pressure upon standing—is present in up to a fifth of healthy, community-dwelling older adults, making it an unreliable sign of volume depletion.3
Clinical assessment of volume status in the elderly is frequently incorrect, yet it is the cornerstone of the conventional model.3
Crack #2: The Polypharmacy Fog
Older adults often take multiple medications, many of which can disrupt sodium balance.
The list of culprits is long and includes some of the most commonly prescribed drugs: thiazide diuretics for blood pressure, certain antidepressants (especially SSRIs), and some pain medications.1
In a patient like Mrs. Vance, who might be on several of these agents, trying to isolate a single “offending drug” is often impossible.
It’s more likely a cumulative effect, a fog of pharmacological inputs that the standard model doesn’t account for.
Crack #3: The Web of Comorbidities
Chronic diseases are the norm in geriatrics, and many of them directly interfere with fluid and sodium regulation.
Congestive heart failure, chronic kidney disease, liver disease, and even lung infections can all cause or contribute to hyponatremia.1
These conditions create complex, overlapping pictures that defy simple categorization into one of the three volume boxes.
A patient can have underlying heart failure (hypervolemic tendency) but also be dehydrated from poor intake (hypovolemic tendency).
Forcing them into a single category is a dangerous oversimplification.
Crack #4: The “Asymptomatic” Myth
Perhaps the most dangerous crack in the conventional model is the idea that mild, chronic hyponatremia (with sodium levels between 125-134 mEq/L) is “asymptomatic.” While it may not cause seizures or coma, a mountain of evidence now shows it is profoundly symptomatic in older adults.
It causes subtle but significant deficits in attention and cognition and impairs gait and balance, dramatically increasing the risk of falls.4
Mrs. Vance’s confusion wasn’t just a baseline symptom of her age; it was an active, dangerous manifestation of her electrolyte disorder, a warning sign I had failed to fully appreciate.
This realization leads to a fundamental shift in perspective.
Hyponatremia in the elderly isn’t just a simple electrolyte disorder.
It behaves like a classic geriatric syndrome, similar to falls, delirium, or frailty.
Geriatric syndromes are defined by having multiple contributing factors, involving impairments across multiple organ systems, and leading to functional decline.
This is a perfect description of hyponatremia in older adults.
Viewing it this way forces us to abandon the simplistic flowchart and adopt the more holistic, comprehensive approach required for any geriatric syndrome.
Part II: The Engineer’s Epiphany: A New Way of Seeing
In the weeks after Mrs. Vance’s fall, I buried myself in research, desperate for a better framework.
The breakthrough came from an unlikely place: the field of engineering.
I stumbled upon the principles of control theory, which describes how systems—from cruise control in a car to a thermostat in a house—maintain stability in a changing environment.23
It was a perfect analogy for the body’s own process of
homeostasis, its constant effort to maintain a stable internal environment in a state of dynamic equilibrium.25
Suddenly, I saw the problem in a new light.
The body’s fluid and sodium balance isn’t a static pool to be measured; it’s a sophisticated, dynamic control system.
Imagine the system that regulates the temperature in your home.
It has one goal: to keep the temperature stable at your desired set point.
The body’s fluid control system has a similar goal: to keep the concentration of solutes in your blood (the osmolality, largely determined by sodium) within a very narrow, life-sustaining range.2
This Homeostatic Control System has several key components:
- The Thermostat (The Controller): This is the hypothalamus in the brain. It acts as the central command, producing Antidiuretic Hormone (ADH), also known as vasopressin. ADH is the key signal that tells the body to either conserve or get rid of water.2
- The Temperature Sensors (The Sensors): The body has two main types of sensors that feed information to the hypothalamus. Osmoreceptors constantly measure the blood’s salt concentration, while baroreceptors measure blood pressure and volume.27
- The Furnace & A/C (The Actuators): These are the components that carry out the controller’s commands. The primary actuators are the kidneys, which can retain or excrete water based on ADH levels, and the thirst mechanism, which prompts us to drink more water.27
- Open Windows & Drafts (The Perturbations): These are all the external and internal factors that disrupt the system and challenge its stability. This includes medications, chronic diseases, poor diet, pain, and emotional stress.1
This analogy was my epiphany.
It fundamentally shifted the clinical goal.
The old goal was to “correct the sodium level.” The new goal is to “diagnose the malfunctioning system.” Instead of just looking at the number on a lab report, I was now forced to ask a series of engineering questions: Are the sensors working correctly? Is the controller getting bad information? Are the actuators broken or inefficient? And most importantly, what external perturbations are throwing the whole system into disarray?
Thinking like an engineer protects you from making critical errors.
Giving saline (turning up the heat) to a patient whose “furnace” (kidneys) is failing or whose “thermostat” (ADH system) is stuck on “cool” because of a drug is not only ineffective but can be dangerous.
This systems-based approach provides a logical, structured framework for investigation that is perfectly suited to the multifactorial complexity of geriatric medicine.
Part III: The Homeostatic Control System: A Geriatric-Focused Framework
Using this new paradigm, we can build a more robust and safer approach to managing hyponatremia in older adults.
It involves systematically evaluating each component of the control system.
Pillar 1: Reading the Sensors (The Diagnostic Deep Dive)
In older adults, the system’s sensors are often faulty.
The thirst mechanism is frequently blunted, meaning an older person may not feel thirsty even when they are dehydrated.21
At the same time, the osmoreceptors that trigger ADH release can become
hypersensitive, leading to an exaggerated water-retaining response to even minor stimuli.32
To get an accurate reading of the system’s status, a comprehensive lab panel is non-negotiable.
This moves us beyond the unreliable physical exam and gives us a clear “diagnostic dashboard.”
Table 1: The Geriatric Hyponatremia Diagnostic Dashboard
| Test | Normal Range | What It Tells the Systems Engineer (Geriatric Interpretation) |
| Serum Osmolality | 275–295 mOsm/kg | Is this a true controller problem? A low value (<275) confirms true hypotonic hyponatremia, where there’s too much water for the amount of solute. If normal or high, it’s not a water balance issue (e.g., pseudohyponatremia from high protein/lipids or high glucose).15 |
| Urine Osmolality | Varies | Is the controller (ADH) ON or OFF? A value >100 mOsm/kg means the ADH system is active and telling the kidneys to retain water. This is “inappropriate” when serum osmolality is low. A value <100 mOsm/kg suggests ADH is suppressed, and the problem is likely excessive water intake (e.g., psychogenic polydipsia).16 |
| Urine Sodium | >20 mEq/L | What kind of signal are the volume sensors sending? In a patient with active ADH, a urine sodium >30 mmol/L suggests the body thinks it has enough or too much volume (as in SIADH or with diuretic use). A value <20-30 mmol/L suggests the body is trying to conserve volume (as in true dehydration or heart failure).12 |
| Serum Uric Acid | 4.0–8.5 mg/dL (men), 2.7–7.3 mg/dL (women) | Is this a clue for SIADH? In SIADH, water retention dilutes the blood and increases uric acid excretion. A low serum uric acid (<4 mg/dL) is a strong supporting clue for SIADH.12 |
| BUN / Creatinine | Varies | How well are the actuators (kidneys) working? Elevated levels indicate chronic kidney disease or acute kidney injury, which impairs the ability to excrete water. Low BUN can be a sign of poor nutrition or SIADH.33 |
Pillar 2: Troubleshooting the Controller (Finding the True Perturbations)
In nearly all cases of true hyponatremia, the ADH controller is active when it should be off.
The critical question is why.
While we often label this as SIADH, this is a diagnosis of exclusion.16
In geriatrics, our first job is to hunt for the perturbations that are fooling the controller into action.
Table 2: A Geriatrician’s Guide to Common System Perturbations
| Perturbation | Mechanism of Disruption (Control System Analogy) | Initial Management Step |
| Thiazide Diuretics (e.g., Hydrochlorothiazide) | Increases renal salt loss, triggering volume sensors and activating the ADH controller. May also directly affect kidney water handling.1 | Stop the medication and switch to an alternative if needed. |
| Antidepressants (especially SSRIs, SNRIs) | Can directly stimulate the hypothalamus (controller) to release ADH inappropriately.12 | Stop or switch to a lower-risk agent (e.g., bupropion) after consulting with the prescribing physician.12 |
| Heart Failure, Cirrhosis | Reduced effective circulating blood volume is detected by baroreceptors (sensors), which send a powerful “we are dehydrated” signal to the ADH controller, causing water retention despite total body fluid overload.1 | Optimize treatment of the underlying disease. Use loop diuretics and fluid/salt restriction. |
| “Tea and Toast” Syndrome (Low Solute Intake) | Provides insufficient solutes (protein, salt) for the kidneys (actuators) to use to create urine and excrete free water. The system is “water-logged” because it lacks the materials to bail itself out.5 | Engage a clinical dietitian to increase protein and solute intake safely.37 |
| Pain, Nausea, Stress | These are potent non-osmotic stimuli that can directly trigger the hypothalamus (controller) to release ADH, independent of fluid status.1 | Treat the underlying pain, nausea, or source of stress. |
Pillar 3: Assessing the Actuators (The Aging Kidney and the Risk of Correction)
The final piece of the puzzle is the machinery itself.
The “senescent kidney” of an older adult is a less efficient actuator.
With age, the glomerular filtration rate (GFR) declines, and the kidneys’ ability to manage large shifts in water and salt is impaired.12
This has profound implications for treatment.
The most critical safety concern in managing hyponatremia is the risk of correcting the sodium level too quickly.
When hyponatremia develops over days or weeks (chronic hyponatremia), the brain adapts.
It protects itself from swelling by getting rid of some of its internal solutes.14
If we then rapidly raise the blood sodium level with aggressive treatment, we create a new osmotic imbalance.
Water is pulled out of the now-adapted brain cells too quickly, causing them to shrink and leading to a devastating neurological injury called
osmotic demyelination syndrome (ODS), which can cause permanent disability or death.13
Therefore, the golden rules of correction are paramount:
- In chronic hyponatremia, the serum sodium should not be corrected by more than 8-10 mEq/L in the first 24 hours, and no more than 18 mEq/L in 48 hours.2
- In patients at high risk for ODS (e.g., those with malnutrition, alcoholism, or very low initial sodium levels), the target should be even more conservative: 4-6 mEq/L per 24 hours.12
Part IV: Re-Calibrating the System: A Success Story
Armed with this new framework, my approach to hyponatremia changed forever.
Consider the case of Mr. Chen, an 88-year-old man whose daughter brought him in for increasing lethargy and confusion.
On paper, he looked just like Mrs. Vance.
His sodium was 122 mEq/L.
The old me would have started down the same flawed path.
The new me started thinking like an engineer.
Step 1: Reading the Sensors & Dashboard. I ordered the full diagnostic panel.
The results confirmed true hypotonic hyponatremia (low serum osmolality).
His urine osmolality was high, meaning his ADH controller was on.
His urine sodium was also elevated, and his uric acid was low.
This pointed away from simple dehydration and toward a state of inappropriate water retention.
Step 2: Troubleshooting the Controller & Perturbations. Instead of stopping at a simple SIADH diagnosis, I dug for the why.
- Medication Review: Mr. Chen was on hydrochlorothiazide for hypertension—a major known perturbing factor.3
- Nutritional History: His daughter mentioned his appetite had been poor since his wife passed away six months prior. He was subsisting on simple meals—another check for low solute intake, or “Tea and Toast” syndrome.7
- Comorbidity Assessment: A careful exam and review of his records suggested his chronic heart failure was not optimally managed, contributing a hypervolemic element to the picture.1
The diagnosis wasn’t one thing.
It was a classic geriatric “perfect storm”: Thiazide-induced, low-solute-intake-exacerbated hyponatremia in the setting of sub-optimally controlled heart failure. This was a nuanced diagnosis the old flowchart could never produce.
Step 3: Assessing the Actuators & Planning a Safe Intervention. I noted his age and his moderately reduced kidney function.
This told me any intervention had to be gentle and slow.
Based on the systems diagnosis, the treatment plan was logical and multi-pronged:
- Remove the Primary Perturbation: We discontinued the hydrochlorothiazide.3
- Optimize the Comorbidity: We switched him to a loop diuretic (furosemide), which is more effective for his heart failure and less likely to cause hyponatremia in the setting of reduced kidney function.2
- Address the Nutritional Deficit: We involved a clinical dietitian to supplement his diet with palatable, nutrient-dense foods and shakes to increase his protein and solute load.37
- Gentle Fluid Management: We instituted a mild fluid restriction of 1.5 liters per day, recognizing that his problem wasn’t just excess water but also a lack of solutes.6
Over the next few days, Mr. Chen made a gradual but steady recovery.
His sodium level rose slowly and safely.
His confusion cleared.
He was discharged home to his daughter’s care, alert and stable—a stark contrast to the tragic outcome that befell Mrs. Vance.
Conclusion: From Physician to Systems Engineer
The journey from Mrs. Vance’s fall to Mr. Chen’s recovery was a transformation in my own practice.
It taught me that in the complex, interconnected world of geriatric medicine, we must evolve.
We cannot be mere technicians who chase and correct numbers on a lab report.
We must become thoughtful systems engineers who diagnose and gently nudge complex, aging biological systems back toward equilibrium.
The “wisdom of the body” that physiologist Walter Cannon described is still present in our older patients, but its signals can be faint, distorted, or contradictory.23
Our job is to learn how to listen to the entire system, to understand its unique frailties, and to intervene with the wisdom, patience, and humility that our patients deserve.
This is the art and the science of modern geriatric care.
Works cited
- Hyponatremia – Endocrine and Metabolic Disorders – Merck Manual Professional Edition, accessed on August 14, 2025, https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/electrolyte-disorders/hyponatremia
- Diagnosis and Management of Sodium Disorders: Hyponatremia and Hypernatremia | AAFP, accessed on August 14, 2025, https://www.aafp.org/pubs/afp/issues/2015/0301/p299.html
- Management of hyponatraemia in older people: old threats and new opportunities – PMC, accessed on August 14, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC4110800/
- Hyponatremia: Special Considerations in Older Patients – ResearchGate, accessed on August 14, 2025, https://www.researchgate.net/publication/272644924_Hyponatremia_Special_Considerations_in_Older_Patients
- [PDF] Hyponatremia in the elderly: challenges and solutions | Semantic Scholar, accessed on August 14, 2025, https://www.semanticscholar.org/paper/Hyponatremia-in-the-elderly%3A-challenges-and-Filippatos-Makri/32d8d75b60c80776cf419f06781ca85651a62622
- How does Tea and Toast Syndrome lead to euvolemic hyponatremia? – Dr.Oracle, accessed on August 14, 2025, https://www.droracle.ai/articles/64198/how-does-tea-and-toast-syndrome-lead-to-euvolemic-hyponatremia
- Tea and toast syndrome – Wikipedia, accessed on August 14, 2025, https://en.wikipedia.org/wiki/Tea_and_toast_syndrome
- Management of hyponatremia – PMC, accessed on August 14, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC4016091/
- Association of hyponatremia with outcomes after geriatric trauma: a systematic review and meta-analysis, accessed on August 14, 2025, https://tsaco.bmj.com/content/10/1/e001562
- Management of hyponatremia in older people: Old threats and new opportunities, accessed on August 14, 2025, https://www.researchgate.net/publication/264429763_Management_of_hyponatremia_in_older_people_Old_threats_and_new_opportunities
- Hyponatremia: Special Considerations in Older Patients – MDPI, accessed on August 14, 2025, https://www.mdpi.com/2077-0383/3/3/944
- Hyponatremia in the elderly: challenges and solutions – PMC, accessed on August 14, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC5694198/
- Management of hyponatremia – Deranged Physiology, accessed on August 14, 2025, https://derangedphysiology.com/main/required-reading/electrolyte-disorders/Chapter-539/management-hyponatremia
- The Role of Nurses in Managing Severe Hyponatremia and Preventing Central Pontine Myelinolysis – Currents, accessed on August 14, 2025, https://currents.neurocriticalcare.org/Leading-Insights/Article/the-role-of-nurses-in-managing-severe-hyponatremia-and-preventing-central-pontine-myelinolysis
- Management of hyponatremia: Providing treatment and avoiding harm – Cleveland Clinic Journal of Medicine, accessed on August 14, 2025, https://www.ccjm.org/content/ccjom/77/10/715.full.pdf
- Hyponatremia – StatPearls – NCBI Bookshelf, accessed on August 14, 2025, https://www.ncbi.nlm.nih.gov/books/NBK470386/
- Hyponatremia: Causes, Symptoms, Diagnosis & Treatment – Cleveland Clinic, accessed on August 14, 2025, https://my.clevelandclinic.org/health/diseases/17762-hyponatremia
- Low blood sodium in older adults: A concern? – Mayo Clinic, accessed on August 14, 2025, https://www.mayoclinic.org/diseases-conditions/hyponatremia/expert-answers/low-blood-sodium/faq-20058465
- Hyponatremia – Symptoms and causes – Mayo Clinic, accessed on August 14, 2025, https://www.mayoclinic.org/diseases-conditions/hyponatremia/symptoms-causes/syc-20373711
- Hyponatremia (Low Level of Sodium in the Blood) – Hormonal and Metabolic Disorders, accessed on August 14, 2025, https://www.msdmanuals.com/home/hormonal-and-metabolic-disorders/electrolyte-balance/hyponatremia-low-level-of-sodium-in-the-blood
- Electrolyte Balance in the Elderly: Challenges and Management – Longdom Publishing, accessed on August 14, 2025, https://www.longdom.org/open-access/electrolyte-balance-in-the-elderly-challenges-and-management-110536.html
- (PDF) Tea and Toast Syndrome: A Case Report – ResearchGate, accessed on August 14, 2025, https://www.researchgate.net/publication/384963124_Tea_and_Toast_Syndrome_A_Case_Report
- Clarifying the Roles of Homeostasis and Allostasis in Physiological Regulation – PMC, accessed on August 14, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC4166604/
- Biological Control Systems: Systems Biology of Diseases and the …, accessed on August 14, 2025, https://ceat.okstate.edu/che/site_files/docs/babatunde-a-ogunnaike.pdf
- www.britannica.com, accessed on August 14, 2025, https://www.britannica.com/science/dynamic-equilibrium-biology#:~:text=If%20homeostasis%20is%20successful%2C%20life%20continues%3B%20if%20unsuccessful%2C%20disaster,yet%20relatively%20uniform%20conditions%20prevail.
- Homeostasis – Wikipedia, accessed on August 14, 2025, https://en.wikipedia.org/wiki/Homeostasis
- Electrolytes in the Aging – PMC, accessed on August 14, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC2901254/
- Homeostasis and Feedback Loops | Anatomy and Physiology I – Lumen Learning, accessed on August 14, 2025, https://courses.lumenlearning.com/suny-ap1/chapter/homeostasis-and-feedback-loops/
- Aging and disturbances of thirst and fluid balance – PubMed, accessed on August 14, 2025, https://pubmed.ncbi.nlm.nih.gov/2406645/
- Tubuloglomerular Feedback and the Control of Glomerular Filtration Rate | Physiology, accessed on August 14, 2025, https://journals.physiology.org/doi/10.1152/nips.01442.2003
- Hyponatremia: practical considerations in the acute geriatric setting – PAGEPress, accessed on August 14, 2025, https://www.pagepressjournals.org/gc/article/view/11711/11895
- Hyponatremia in the Elderly: Risk Factors, Clinical Consequences, and Management | Consultant360, accessed on August 14, 2025, https://www.consultant360.com/articles/hyponatremia-elderly-risk-factors-clinical-consequences-and-management
- Chapter 16: Disorders of Serum Sodium Concentration in the Elderly Patient – American Society of Nephrology, accessed on August 14, 2025, https://www.asn-online.org/education/distancelearning/curricula/geriatrics/Chapter16.pdf
- View of Approach To Hyponatremia In The Elderly | BMH Medical Journal – ISSN 2348–392X, accessed on August 14, 2025, https://www.babymhospital.org/BMH_MJ/index.php/BMHMJ/article/view/248/544
- Hyponatremia and Hypernatremia in the Elderly – AAFP, accessed on August 14, 2025, https://www.aafp.org/pubs/afp/issues/2000/0615/p3623.html
- Approach to the Patient: Hyponatremia and the Syndrome of Inappropriate Antidiuresis (SIAD) – PMC – PubMed Central, accessed on August 14, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC9282351/
- Dietary essentials for sodium and fluid imbalance | Dietitians On Demand Blog, accessed on August 14, 2025, https://dietitiansondemand.com/dietary-essentials-for-sodium-and-fluid-imbalance/
- Tea and Toast Syndrome: What is it, Symptoms, and How to Prevent – Crossroads Hospice, accessed on August 14, 2025, https://www.crossroadshospice.com/hospice-palliative-care-blog/2022/january/27/prevent-tea-toast-syndrome/
- Fluid and electrolyte homeostasis in the elderly: Physiological changes of ageing and clinical consequences – Johns Hopkins University, accessed on August 14, 2025, https://pure.johnshopkins.edu/en/publications/fluid-and-electrolyte-homeostasis-in-the-elderly-physiological-ch-4
- Principles of Management of Severe Hyponatremia – American Heart Association Journals, accessed on August 14, 2025, https://www.ahajournals.org/doi/10.1161/jaha.112.005199
- Diagnosis and Treatment of Hyponatremia: Compilation of the Guidelines – PMC, accessed on August 14, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC5407738/
- Hyponatremia and malnutrition: a comprehensive review – PMC, accessed on August 14, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10961272/