Table of Contents
The Formula That Failed Me – An Introduction
I remember the feeling with perfect clarity.
It was the third month of my internal medicine residency, and the emergency department was its usual symphony of controlled chaos.
In the middle of it all, I felt a sense of command I hadn’t known just weeks earlier.
Tucked into my white coat pocket was a small, dog-eared handbook, its pages filled with the algorithms and formulas that were the bedrock of my new authority.
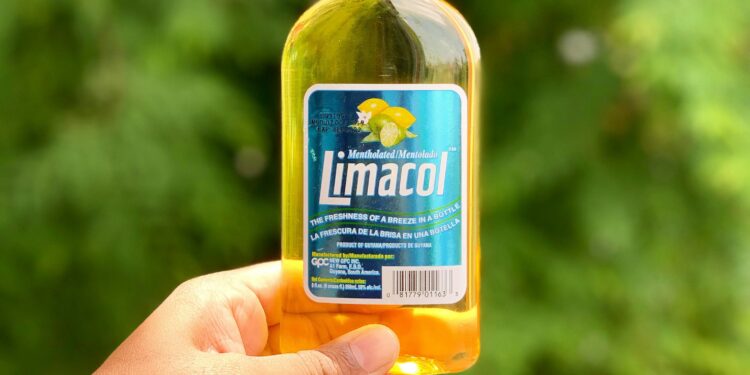
Of all these trusted tools, none felt more solid, more reassuringly concrete, than the formula for “corrected sodium” in a hyperglycemic patient.
In the world of acute medicine, where decisions are made in minutes and the stakes are life and death, simplicity is seductive.
The formula was beautiful in its simplicity: for every 100 mg/dL that a patient’s glucose was above 100, you simply added 1.6 mEq/L to their measured sodium level.1
This single calculation promised to cut through the fog of a complex metabolic crisis, to give you a “true” number to guide your therapy.
It was a piece of dogma, passed down from attending physicians to residents, unquestioned and universally applied.
It felt like a law of physiology, as immutable as gravity.
This reliance on heuristics is a natural defense against the overwhelming cognitive load of a busy hospital.
We are trained to recognize patterns and apply established protocols, and these formulas become our cognitive anchors in the storm.3
They seem to offer a linear, predictable path through the non-linear chaos of human biology.
For a time, I believed in that predictability.
I believed that if I just followed the formula, I could master the dangerous dance between sugar and salt that plays out in patients with diabetic ketoacidosis (DKA) or hyperosmolar hyperglycemic state (HHS).
I had not yet learned that the most dangerous number in medicine isn’t the one that’s wrong, but the one that’s blindly trusted.
A single case, a patient whose body refused to follow the textbook, would shatter that illusion and force me to question the very foundations of my training.
The Physiological Tug-of-War: Why High Sugar Creates a Sodium Mirage
Before I tell you about that patient, you must first understand the battlefield.
The relationship between sodium and glucose in a hyperglycemic crisis is not a simple one-way street; it’s a violent physiological tug-of-war, with two powerful and opposing forces ripping the body’s water balance in opposite directions.
The measured sodium value a clinician sees on a lab report is merely a snapshot of this dynamic conflict, an artifact of the battle rather than a true measure of the body’s state.
To understand this, imagine the body’s fluid compartments as two massive, interconnected reservoirs.
The first is the Intracellular Fluid (ICF) reservoir, containing all the water inside our trillions of cells.
The second is the Extracellular Fluid (ECF) reservoir, which includes the blood plasma.
These two reservoirs are separated by a vast, semi-permeable dam—the collective membranes of all our cells.
Water can pass freely across this dam, but solutes like sodium and glucose cannot.
The first force in this tug-of-war is The Dilution Effect.
When a patient develops severe hyperglycemia, a massive amount of glucose—an osmotically active solute—is suddenly dumped into the ECF reservoir.5
This dramatically increases the osmolality, or solute concentration, of the extracellular fluid.
The body, in its relentless pursuit of equilibrium, responds immediately.
Water rushes across the cellular dam, moving from the less concentrated ICF into the more concentrated ECF to try and equalize the pressure.6
This flood of intracellular water into the bloodstream dilutes everything in it, including sodium.
The result is a laboratory finding of hyponatremia, or low sodium.8
This is often called dilutional hyponatremia.
But this is only half the story.
At the exact same time, a second, opposing force is at work: The Dehydration Effect.
The kidneys have a limit to how much glucose they can reabsorb from the filtered urine.
When blood glucose levels exceed this threshold (typically around 180–200 mg/dL), the transporters in the kidney tubules become saturated, and glucose begins to spill into the urine—a condition called glycosuria.6
This glucose in the urine acts like a powerful osmotic magnet, pulling huge volumes of water along with it.
This process, known as osmotic diuresis, is like opening a massive sluice gate at the far end of the ECF reservoir.
The body begins to lose staggering amounts of fluid.
Crucially, this diuresis causes a loss of water that is far in excess of the loss of sodium.6
This loss of “free water” should, by itself, cause the sodium concentration in the remaining blood to rise, leading to hypernatremia.
So, a clinician is faced with a paradox.
The patient is almost always profoundly dehydrated, having lost liters of free water, a state that should cause high sodium.10
Yet, the lab report often shows low sodium because of the massive osmotic fluid shift from the cells.
The final measured sodium level is the confusing net result of the inward rush of diluting water and the outward drain of dehydrating diuresis.
It depends on the severity and duration of the hyperglycemia, the patient’s ability to drink water, and the degree of renal water loss.6
This is the central physiological problem that the simple “corrected sodium” formula attempts to solve.
And it is in the treacherous gap between this complex reality and the formula’s oversimplification that clinical disaster awaits.
A Patient on the Brink – When the Formula Led to Danger
He was an 82-year-old man brought in by his family for “not acting right.” He had a history of poorly controlled type 2 diabetes, and for the past week, he’d been fighting what seemed like a simple cold.
He was lethargic, his mouth was bone-dry, and his skin had the texture of parchment—all classic signs of profound dehydration.2
The fingerstick glucose read “HIGH,” meaning it was over the meter’s 600 mg/dL limit.
The initial lab results from the emergency department confirmed a crisis.
His blood glucose was 850 mg/dL.
His serum sodium was 125 mEq/L.
This was it.
The classic scenario.
I felt a surge of confidence as I pulled out my pen and did the math on a scrap of paper.
The glucose was 750 mg/dL above the 100 mg/dL threshold.
Using the trusted formula:
7.5×1.6=12
Corrected Sodium = Measured Sodium + Correction
Corrected Sodium = 125+12=137 mEq/L
My conclusion was swift and certain.
“His sodium is basically normal,” I announced to the team.
“The core problem is severe dehydration.
The protocol for a normal corrected sodium in HHS is to use 0.45% saline to replace his free water deficit”.2
We started an intravenous (IV) line and began the hypotonic fluids, along with a cautious insulin infusion.
I expected to see improvement within hours.
Instead, his neurological status worsened.
His lethargy deepened into a stupor, and then, terrifyingly, his right arm began to twitch—a focal seizure.10
A wave of cold panic washed over me.
This wasn’t supposed to happen.
I had followed the protocol.
I had trusted the formula.
What had I missed?
The attending physician, a man with decades of experience, came to the bedside.
He looked at the patient, then at the labs, then at my face.
He asked a question I hadn’t even thought to consider.
“What’s his lipid panel look like?”
It was a jarring question, but we checked.
The patient’s triglycerides were astronomically high, over 2000 mg/dL—a common finding in uncontrolled diabetes.5
My attending explained the concept of
pseudohyponatremia.
The standard lab method for measuring sodium, an indirect ion-selective electrode (ISE), involves diluting the blood sample first.
If the sample contains a large volume of lipids or proteins, this non-aqueous “solid” phase displaces the water-containing “aqueous” phase where the sodium actually resides.
This leads to an artificially low sodium reading.14
However, a direct ISE, like the one in a blood gas analyzer, measures sodium activity in the undiluted sample and is not affected by this artifact.16
We ran an arterial blood gas.
The sodium on the gas machine came back at 135 mEq/L—a full 10 points higher than the value I had used for my calculation.
The foundation of my entire treatment plan had been quicksand.
My initial error of dogma—blindly trusting a single lab value—had led to a cascade of potential judgment errors.
The patient’s clinical picture was not a single, clean problem but a messy, confounding reality.
The formula hadn’t just failed; it had actively misled me, and the consequences were playing out in my patient’s worsening condition.
The Epiphany – Our Bodies Are Not Simple Calculators
That night, after my shift ended, I couldn’t rest.
The near-miss haunted me.
I went to the hospital library and started pulling up the primary literature, digging past the simplified summaries in textbooks to find the original research.
That’s when I found the 1999 study by Hillier and colleagues, and as I read it, the ground shifted beneath my feet.1
The researchers had experimentally induced acute hyperglycemia in healthy volunteers to directly measure the effect on serum sodium.
Their findings were a bombshell that dismantled the dogma I had so faithfully followed.
First, they found that the average decrease in sodium was not 1.6, but 2.4 mEq/L for every 100 mg/dL increase in glucose.18
The classic formula was underestimating the effect by 50%.
But the most crucial finding was this: the relationship was not linear.
The osmotic pull of glucose on water becomes disproportionately stronger at extreme concentrations.
Up to a glucose level of 400 mg/dL, the old 1.6 factor worked reasonably well.
But for glucose levels above 400 mg/dL, the researchers found a much better correction factor was 4.0.18
I felt a jolt of adrenaline as I grabbed my pen and recalculated my patient’s sodium, this time with the new, more accurate model.
His glucose was 850 mg/dL, well into the non-linear range.
Using the initial measured sodium of 125 mEq/L (ignoring the pseudohyponatremia for a moment to see the formula’s raw error):
7.5×4.0=30
Corrected Sodium = 125+30=155 mEq/L
The number stared back at me from the page.
155 mEq/L.
My patient wasn’t normonatremic.
He was profoundly, dangerously hypernatremic.
The choice of hypotonic saline had been correct, but my reasoning was catastrophically flawed.
If his measured sodium had been just a bit higher—say, 135 mEq/L (the value from the blood gas)—my old calculation would have yielded a corrected sodium of 147 mEq/L (135+12), still in the “high-normal” range.
But the true corrected sodium would have been 165 mEq/L (135+30), a life-threatening level of hypernatremia where fluid management must be exquisitely careful to avoid cerebral injury.
The “Interconnected Reservoirs” analogy clicked into place with new clarity.
The 1.6 formula works only when the system is under mild stress.
But at extreme glucose levels, the system breaks.
The osmotic gradient becomes overwhelming, the cellular dam is under immense pressure, and the relationship between glucose and water movement is no longer linear and predictable.
The simple formula is designed for a scenario where it isn’t critically needed, and it fails spectacularly in the very crisis it’s meant to solve.
My epiphany was not just that the formula was wrong.
It was that true clinical expertise isn’t about memorizing rules; it’s about understanding the principles that govern when those rules break down.
It was a shift from a rule-based mindset to a principle-based one.
The Modern Clinician’s Playbook for the Sugar-Salt Dance
That experience forced me to abandon dogma and develop a new, principle-based playbook for managing these incredibly fragile patients.
It is not a rigid checklist but a dynamic algorithm built on a cycle of assessment, wise calculation, precise action, and constant reassessment.
Step 1: Assess the Whole Picture, Not Just the Sodium
Before you even think about a formula, you must assess the patient.
- Evaluate Volume Status: Every patient in DKA or HHS is volume depleted, often profoundly. Look for signs of severe dehydration: poor skin turgor, dry mucous membranes, tachycardia, and hypotension.2 Fluid resuscitation to restore intravascular volume and organ perfusion is always the first priority.3
- Differentiate DKA vs. HHS: While treatment principles overlap, it’s important to distinguish them. DKA is characterized by significant ketosis and acidosis, while HHS involves more extreme hyperglycemia and hyperosmolality with minimal ketosis.10 Remember that up to a third of patients present with features of both conditions.10
- Actively Suspect the Artifact: In any patient with hyponatremia and a hyperglycemic crisis, you must consider the possibility of confounding pseudohyponatremia. Check a lipid panel and, most importantly, compare the sodium from the chemistry panel (an indirect ISE) with the sodium from a blood gas analyzer (a direct ISE). A significant discrepancy strongly suggests an artifact that will invalidate any correction formula if not accounted for.14
Step 2: Calculate with Wisdom, Not Dogma
Once you have a reliable measured sodium value, use a correction model that respects the non-linear physiology.
The classic formula should be retired for all but the mildest cases.
| Correction Model | The Formula | Clinical Context & Glucose Range | Key Limitations & Clinical Pearls |
| Katz (The Classic) | Add 1.6 mEq/L for every 100 mg/dL glucose > 100 | Mild-to-moderate hyperglycemia (Glucose < 400 mg/dL) | Dangerously underestimates true sodium in severe hyperglycemia. Should be considered obsolete for critically ill patients.1 |
| Hillier (The Modern Average) | Add 2.4 mEq/L for every 100 mg/dL glucose > 100 | A better overall estimate across a range of glucose values. | Still a linear approximation of a non-linear process. May be less accurate at the highest extremes compared to the non-linear approach.1 |
| Hillier (The Non-Linear) | Add 4.0 mEq/L for every 100 mg/dL glucose > 400 | Severe hyperglycemia (Glucose > 400 mg/dL). The most accurate model for critically ill DKA/HHS patients. | Requires a two-step thought process but best reflects the underlying physiology. This is the expert’s choice in a crisis.1 |
Step 3: Resuscitate with Precision
The choice of IV fluid is one of the most critical decisions you will make.
It must be based on the wisely calculated corrected sodium.
- If the corrected sodium is low (<135 mEq/L), the patient has a true sodium deficit. Use 0.9% NaCl (Isotonic Saline).
- If the corrected sodium is normal or high (≥135 mEq/L), the patient has a profound free water deficit. Use 0.45% NaCl (Hypotonic Saline) to replace that free water without providing excess sodium.2
Step 4: The Art of the Slow Correction
The brain, in an effort to protect itself from the severely hyperosmolar state of the blood, generates its own intracellular solutes called “idiogenic osmoles.” This prevents brain cells from shrinking and dehydrating.
If you correct the blood’s osmolality too quickly with fluids and insulin, you create a new osmotic gradient where the blood becomes hypotonic relative to the brain cells.
Water then rushes into the brain, causing life-threatening cerebral edema.11
- Monitor relentlessly: Check electrolytes, glucose, and osmolality every 1-2 hours initially.
- Aim for a gentle decline: The goal is a slow, steady reduction in plasma osmolality. The rate of sodium correction should not exceed 10 mEq/L in the first 24 hours.5
- Be dynamic: Adjust your insulin infusion and fluid rates based on the patient’s response, not a rigid, pre-printed protocol. You are guiding a complex system back to equilibrium, not just hitting a target number.
Conclusion – Beyond the Formula, Toward Wisdom
Years later, I treated another patient, a young woman with newly diagnosed type 1 diabetes who presented in severe D.A. Her glucose was over 900 mg/dL, and her measured sodium was 128 mEq/L.
The old me would have reflexively calculated a corrected sodium of around 141 mEq/L (128+[8×1.6]) and started hypotonic fluids.
But the new me paused.
I followed the playbook.
I confirmed her lipids were normal.
I applied the non-linear correction factor: 128+(8×4.0)=160 mEq/L.
She was severely hypernatremic.
I initiated aggressive resuscitation with isotonic saline first to restore her volume, then transitioned to hypotonic saline, carefully titrating the fluids and insulin while monitoring her labs hourly.
Her osmolality came down slowly and predictably.
Her neurological status improved steadily.
She walked out of the hospital five days later.
That case was the final proof.
The journey through the confusing world of sugar and salt taught me the most important lesson of my career: our role as clinicians is not to be human calculators, blindly applying formulas.
It is to be wise interpreters of the profound physiological stories our patients’ bodies are telling us.
The numbers on the lab report are just the vocabulary.
Understanding the grammar—the principles of physiology, the context of the patient, and the limits of our tools—is what allows us to read the story correctly.
The goal is not just to “correct” a number, but to understand the complex system that produced it, and to guide that system, gently and wisely, back to a state of balance.
Works cited
- Adjusting Sodium Levels in Patients with Hyperglycemia – AAFP, accessed on August 14, 2025, https://www.aafp.org/pubs/afp/issues/1999/1015/p1821.html
- Hyperosmolar Hyperglycemic State (HHS) – Endocrine and Metabolic Disorders – Merck Manual Professional Edition, accessed on August 14, 2025, https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/diabetes-mellitus-and-disorders-of-carbohydrate-metabolism/hyperosmolar-hyperglycemic-state-hhs
- Updates in the Management of Hyperglycemic Crisis – PMC, accessed on August 14, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10012093/
- Hyperglycemic Crises in Adults With Diabetes: A Consensus Report, accessed on August 14, 2025, https://diabetesjournals.org/care/article/47/8/1257/156808/Hyperglycemic-Crises-in-Adults-With-Diabetes-A
- Hyponatremia in Diabetes Mellitus: Clues to Diagnosis and Treatment, accessed on August 14, 2025, https://www.iomcworld.com/open-access/hyponatremia-in-diabetes-mellitus-clues-to-diagnosis-and-treatment-2155-6156-1000560.pdf
- Sugar, Sodium, and Water: A Recipe for Disaster | Annals of the …, accessed on August 14, 2025, https://www.atsjournals.org/doi/full/10.1513/AnnalsATS.202004-360CC
- Corrected sodium levels for hyperglycemia is a better predictor than measured sodium levels for clinical outcomes among patients with extreme hyperglycemia, accessed on August 14, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC7478195/
- Hyponatremia vs. Hyperglycemia: What’s the Difference? – Healthline, accessed on August 14, 2025, https://www.healthline.com/health/hyponatremia-vs-hyperglycemia
- Diabetic Ketoacidosis with Hyponatremia Tension-type Headache and Migraine as – Cermin Dunia Kedokteran, accessed on August 14, 2025, https://cdkjournal.com/index.php/cdk/article/download/866/808/2587
- Hyperosmolar Hyperglycemic State – AAFP, accessed on August 14, 2025, https://www.aafp.org/pubs/afp/issues/2017/1201/p729.html
- Hyperosmolar Hyperglycemic Syndrome – StatPearls – NCBI Bookshelf, accessed on August 14, 2025, https://www.ncbi.nlm.nih.gov/books/NBK482142/
- Diabetic hyperglycemic hyperosmolar syndrome: MedlinePlus Medical Encyclopedia, accessed on August 14, 2025, https://medlineplus.gov/ency/article/000304.htm
- Hypernatremia in Diabetic Ketoacidosis: Rare Presentation and a Cautionary Tale – PMC, accessed on August 14, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC7781561/
- Pseudohyponatremia – StatPearls – NCBI Bookshelf, accessed on August 14, 2025, https://www.ncbi.nlm.nih.gov/books/NBK553207/
- Pseudohyponatremia: Mechanism, Diagnosis, Clinical Associations and Management, accessed on August 14, 2025, https://www.mdpi.com/2077-0383/12/12/4076
- Pseudohyponatremia – Acutecaretesting.org, accessed on August 14, 2025, https://acutecaretesting.org/en/articles/pseudohyponatremia
- An unusual case of hyponatraemia in diabetic ketoacidosis – PMC, accessed on August 14, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC1770770/
- Hyponatremia: evaluating the correction factor for hyperglycemia, accessed on August 14, 2025, https://pubmed.ncbi.nlm.nih.gov/10225241/
- Sugar, Sodium, and Water: A Recipe for Disaster – ATS Journals, accessed on August 14, 2025, https://www.atsjournals.org/doi/pdf/10.1513/AnnalsATS.202004-360CC?download=true
- Hyperglycemic Crises – Endotext – NCBI Bookshelf, accessed on August 14, 2025, https://www.ncbi.nlm.nih.gov/books/NBK279052/
- Hyperglycemic Hyperosmolar State: A Pragmatic Approach to Properly Manage Sodium Derangements – PMC – PubMed Central, accessed on August 14, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC6237920/
- Management of Hyponatremia | AAFP, accessed on August 14, 2025, https://www.aafp.org/pubs/afp/issues/2004/0515/p2387.html